Transsexual Pregnancy
(For Male-to-Female Transsexuals)
Chapters Includes in This Section include:
Finding Love as a Transsexual Woman
Transssexual Women and Sex
Essential Considerations for Transsexual Love
Transsexual Erections Sexual Joy
Cleaning Up Your Act Before Starting on a Love Journey
Early Stage Gender Transition and Love
The Sexual Orientation of Transsexual Women
Sorting Out Your Sexual Orientation as a TS Woman
Transsexual Pregnancy
Marriage and the Transsexual Woman
The Transsexual Mother
Dating and Loving a Man - for Transsexual Women
The Secret to Finding the Perfect Man for Marriage - for TS Women
Lesbian Females with Transsexuals
Trans Lesbians: Love Between Two Transsexual Women
Transsexual Women that Love and Date Straight Females
Post Operative Transsexual Love
"I just want to have a baby..."
Mrs Haynes: “Becoming a mother was the single most amazing moment of my life."
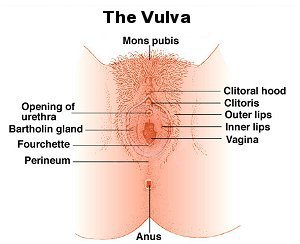
| Medical advances have transformed the lives of transsexual woman since the 1950's. Hormones provide huge physical and mental benefits, whilst with advances in Sex Re-assignment Surgery techniques it has become difficult to distinguish the vulva (external genitalia) of a genetically XY male-to-female (MTF) transsexual women from that of a XX women. An increasing number of transsexual women now lead their lives without their sexual partners and even husband ever suspecting that they were born anything other than a woman. |
|
 One study found that transsexual women are as likely to have reproductive dreams and daydreams as any other women.
One study found that transsexual women are as likely to have reproductive dreams and daydreams as any other women.
Nevertheless, transwomen still cannot bear children due to their lack of internal female reproductive organs. Further, a transsexual woman seeking to have children and be a
mother
faces far more barriers than a genetic XX women in relation to adoption or the use of a surrogate mother.
|
Historically there has been relatively little pressure on the medical profession to aid transsexual women to have children as few have wanted to. But there has been a huge western and age'ist bias to this finding. For example, very few Thai or Brazilian MTF transsexuals (typically transitioning in their early 20's) have sired any children before having SRS. By comparison, more than half of European transsexuals (with a typical transition age in their late 30's or early 40's) have been married at least once, and most of these have had children. But even this is a historic finding, e.g. in 2015 the average age of patents being referred to the UK's NHS gender identity clinics was under 30 after repeated huge annual rises in the number of teenagers - the Sun newspaper
suggested 1000%
. A NHS publication of 2014 quoting an average of age of 42 was probably overtaken by events before it was even printed.
|
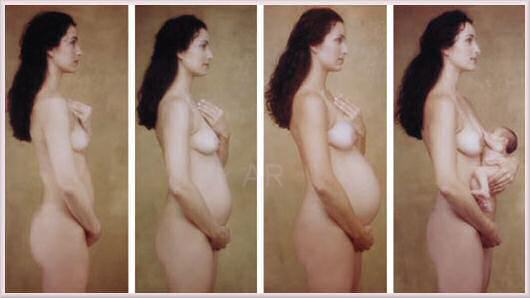
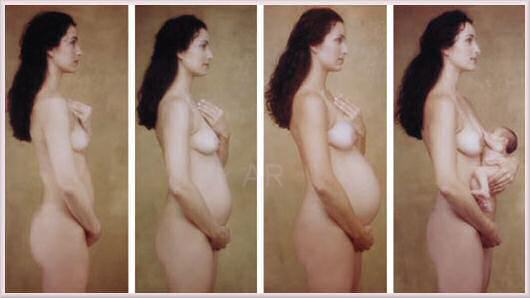
 Famous models and actresses often flaunt their pregnancy in the media
- unfortunately causing distress for some infertile women
Famous models and actresses often flaunt their pregnancy in the media
- unfortunately causing distress for some infertile women

Ayana Tsubaki and
Jenny Hiloudaki
- post-SRS transsexual women 'photo-shopped' as pregnant for advertisements.
|
Some transwomen - typically those who transitioned at very young age (as is becoming increasingly common) - experience extreme broodiness, jealousy of pregnant women, anger at the "unfairness of life" and even clinical depression. Seeing other women having children or even worse complaining about their fertility and worse seeking abortions is often hard to bear. One very frustrated British male-to-female (MTF) transsexual in her 20's said "I just want to be a Mum ... with a pile of kids". The denial of the basic female right to have children and enjoy the wonderful and unique experience of motherhood is a tragic loss for these women - as it is for all infertile women.
|

Transgender woman Nicole Ferri with a security guard, she's faking being pregnant using just a cushion
|
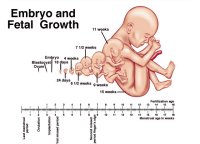
Even if just 1 in 20 transwomen suffers from infertility stress, that is still amounts to tens of thousands of women. However, the situation may eventually improve.... Until 2000 the idea of a genetic male (XY) being pregnant with a baby was still in the realm of science fiction, but since then huge advances in female fertility treatment have made it a real possibility for transsexual women who are prepared to undergo the vital supportive hormone treatment and surgery. It now seems quite possible that a transwoman will give birth by 2020.
|
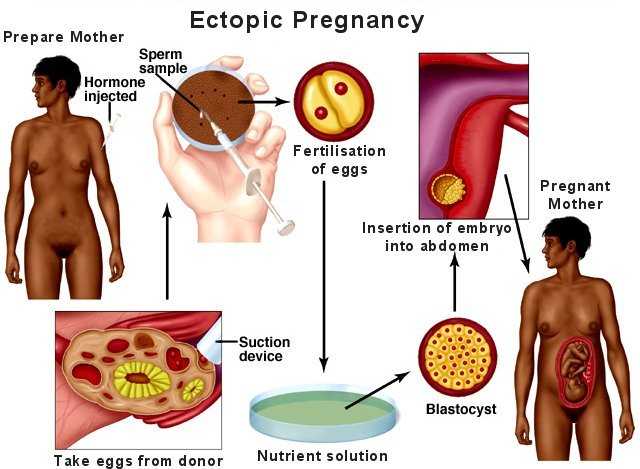
Two potentially viable medical approaches were long ago identified for transsexual women seeking to bear a baby - uterus transplant or ectopic pregnancy. In recent years the former has emerged by far the most practical, but both are discussed below.
|
Female Reproductive Organs
|
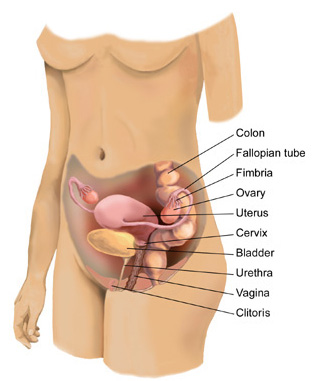
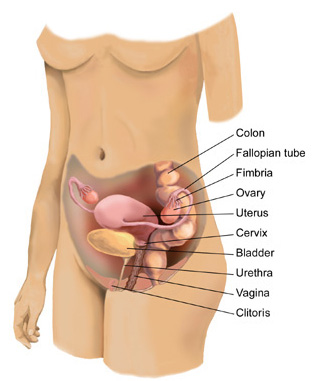
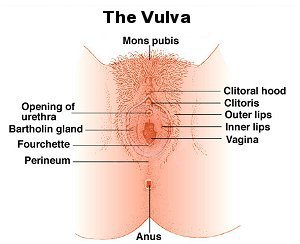
Before going any further it is necessary to consider, very briefly, what are the internal female reproductive organ?
|
The normal female reproductive organs include the vagina (a muscular passage that connects the cervix with the external genital organs - one of which is a sensitive mound of tissue called the clitoris), the cervix (the lower part of the uterus that separates the body of the uterus from the vagina), the uterus (a hollow, muscular structure), the ovaries (two glands that produce certain hormones and contain tissue sacs in which eggs develop), and fallopian tubes (two muscular channels that connect the ovaries with the uterus). Finger-like projections called fimbriae (located at the opening of the fallopian tubes) sweep an egg released from an ovary into the tube where it can be fertilized by sperm before passage in to the uterus (womb) where it may settle and grow in to a baby. Additionally of course, women have a unique secondary sexual characteristic that becomes important after giving birth, their breasts.
|
With modern surgical techniques, if a transsexual woman has had good quality sex re-assignment surgery (SRS), her vulva - including the clitoris and its hood and the opening to the vagina with its lips - should be visually almost indistinguishable from other women. (Scaring is the most common give away in good light). However, the vagina does not lead on to a cervix. Indeed the cervix, uterus, ovaries, fimbria and fallopian tubes are all missing. For the foreseeable future it seems impossible that a transsexual women will be able to have transplanted in to her the full and very complicated reproductive apparatus of a normal fertile woman. Whilst the transplant of some individual organs (e.g. heart or liver) has been possible for decades, transplanting ovaries and fallopian tubes and a uterus - and then establishing ovulation, periods and fertility is far beyond the current state of medical science.
|
|
Uterus Transplants
|
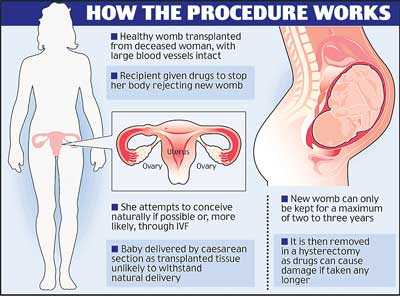
By far the most promising approach that could allow a transsexual woman to become pregnant is a uterus (aka womb) transplant. For decades a huge medical effort was undertaken to transplant a uterus into to a genetically female woman for fertility reasons. In 2014 this led to the first successful full term pregnancies and live births. There is no reason why exactly the same technique cannot used for a genetically male transsexual woman.
|
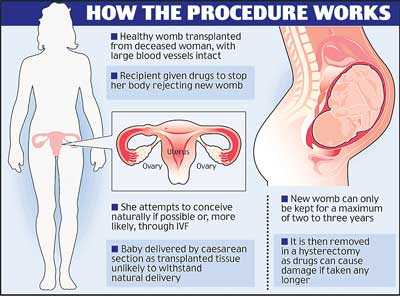
Essentially the transwoman will receive a transplanted womb for at least long enough to her to conceive and give birth by Caesarean section. Ideally this will come from a close female relative (mother or sister), but other donors are possible such as a deceased woman who who used as an organ donor (a 'cadaver' in medical terminology), also a recent development is possibility that a womb could be grown in a laboratory from the transwoman's own cells (see below). This has the huge advantage that possibility of rejection is eliminated, and the uterus can remain in place long term.
|
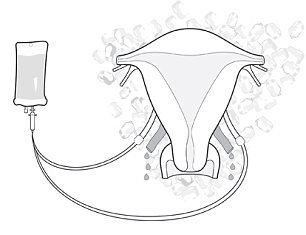
A graphic illustrating how a uterus transplant operation works. The chances of a successful pregnancy are much improved if the transplanted uterus is from a sister, mother or another close relative - the first transsexual woman to bear a child seems likely to come via this route.
|
Eggs from a donor (again, ideally, from a close female relative) will be fertilized by her partner's sperm via the now common IVF technique and placed in the implanted uterus. The sperm could even be her own - from a sample taken and frozen before having SRS. After birth, the uterus would be removed, eliminating the need for the woman to take risky immunity suppression drugs long-term.
|
The baby will need to be delivered by Caesarean section because the transwoman lacks the organs and muscles involved in natural contractions and labour, but this is minor obstacle given that about quarter of all babies are already born by this method in Western Europe, and a third in the USA.
|
For a transsexual woman absolutely determined to start a family, uterine transplants offer some major advantages over surrogacy. The transsexual is gestationally and socially clearly the mother. She can also control lifestyle factors such as smoking and drinking alcohol, and she is the person who takes the health risks associated with every pregnancy.
|
A Brief History of Uterus Transplants
|
Until the 1990's uterus implants were not regarded as a viable approach - experiments with dogs and baboons had been unsuccessful as it was found that great difficulties lie in the fact that complex blood vessels that must be connected. Pregnancy also puts huge strain on these connections, with very dangerous consequences if something was goes wrong. Another major problem when transferring a uterus from one person to another is the possibility of rejection (i.e. the transplanted womb is recognized by the implanted body as being foreign material and "attacked"), especially if that occurred during a pregnancy. The risk of rejection can only be reduced by taking drugs to suppress the immune system and prevent rejection of the transplant, but most of these drugs are harmful to the early fetus development during a pregnancy.
|

It was thus thought that uterus implants must wait either until less intrusive immunology suppression drugs are developed, or until advances in cloning or genetic engineering allows the growth of female reproductive organs that are not "foreign" to the patient. However the concept of short-term uterus implants in order to bear a baby has emerged... creating what has effectively become a competition for the first successful pregnancy via this technique.
|
A
paper
published in the International Journal of Gynecology and Obstetrics in March 2002 claimed that doctors in Saudi Arabia had performed the world's first womb transplant. The operation was on a 26-year-old woman who had lost her own womb because of excessive bleeding after childbirth. The operation used the womb of a 46-year-old woman who needed a hysterectomy, and was performed on 6 April 2000. It was deemed a success by the Saudi doctors but the transplanted womb had to be removed 99 days later when scans revealed a blockage in one of the grafted vessels that cut off blood supply to the uterus. However, the uterus did produce two hormone induced (as would be done in a transsexual woman) menstrual periods before it had to be removed.
|
Researchers now sought better ways of "plumbing in" the transplanted uterus than the Saudi's had used.
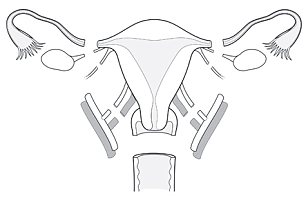
In June 2003 a Swedish team led by Dr Brännström of Sahlgrenska University in Gothenburg, briefed a "European Society of Human Reproduction and Embryology Conference" in Madrid about a new technique where the transplanted womb is attached to two arteries and three veins on each side, with blood primarily coming from the external iliac artery. It would also be attached to the vagina, and to the round and sacral ligaments to hold it in place, but not to the Fallopian tubes - if the woman has those. The woman would not be able to conceive naturally, but would have to have IVF. She would also have to give birth by Caesaeran. The new technique was considered simpler and less risky than most transplant operations as no major blood vessels or vital organs are involved.
|
The donated womb would have to come from a woman with a close genetic match to the recipient in order to minimize the chance of rejection, as the womb does not deteriorate greatly from age it could come come from a post-menopausal woman.
According to Dr Brännström "It could well be a relative. You could get it from your mother. You could give birth to a baby from the uterus that you yourself were birth from." Patients would need to take immunosuppressant drugs to help stop their body rejecting the womb, but researchers believe that modern immunosuppressant drugs do not have any negative effects on a feotus. Also, the drugs would not need to be taken for life, which might result in undesirable long term side-effect. After the woman has had her children, the transplanted womb could be removed.
|
Dr Brännström says that it might be possible to transplant a womb in to transsexual women, allowing them to become pregnant with using donated eggs, though anatomical barriers would have to be overcome. "It should be technically possible, but I don't know if it's ethical. The
pelvis
of men also is not exactly the same shape as the pelvis of women, and that might pose problems."
|

In reaction to news that womb transplants may be imminent, a Hungarian
newspaper
expressed concern about womb peddling and the possibility of "gynecological care that routinely results in women going in for a check-up and only finding out later they've been given a hysterectomy" and "girls from the Hungarian countryside selling their wombs to rich yuppies from New York". Akció means 'for sale (special offer)'.
|
Also in November 2006 Dr Giuseppe Del Priore, from New York Downtown Hospital, said he had been given the go-ahead to carry out a womb transplant operation and claimed to have found a number of potential donors. Dr Del Priore said: "It is cautionary approval but it is approval. If the right patient shows up the [hospital] independent review board has stated we could go-ahead. Technically we are capable of doing it. If we had everything in order we could do it tomorrow." However any would-be patient will have to go through months of counselling and tests before approval - including seeing a psychologist and reconsidering adoption or surrogacy, as well as seeing a pregnancy risk specialist and transplant support team. The organ is likely to be sourced from a dead donor who had previously had a child. They would have to have the same blood group and be immunologically matched.

The long race for the first successful uterus transplant and pregnancy reached another small milestone when in
October 2009
Dr Richard Smith- a consultant gynecological surgeon at Hammersmith Hospital in London - claimed that his teams' research on animals had “cracked” how to ensure a good blood supply to a transplanted womb.
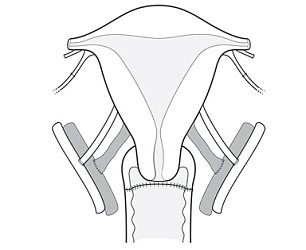
Procedure for the removal of a Uterus from a living donor
|
|
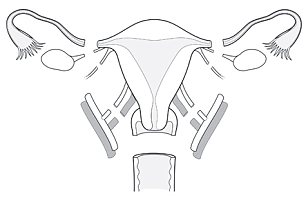
Step 1. The uterus is taken from the donor through an incision in the abdomen and placed on a bed of ice
|
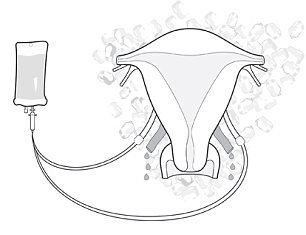
Step 2. The blood vessels to the uterus is flushed with cold preservation solution
|
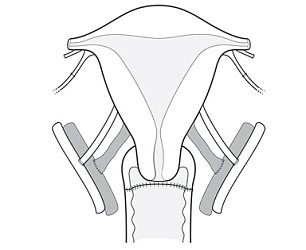
Step 3. The three hour operation of the donor ends after the top of the vagina is sewn up.
|
However the next millstone was reached by the doctors at Akdeniz University Hospital in southern Turkey. On 9th August 2011 they transplanted -in a seven hour operation - a uterus from a woman who had died in a car crash to a genetically XX 21 year old woman, Derya Sert, who was born without a uterus. Micro-surgeon Omer Ozkan, said: "The surgery was a success ... [But] we will be successful when she has her baby. ... For now we are happy that the tissue is living.'
|

|
Mrs Derya Sert
|
Mrs Sert then spent six months in hospital and was given powerful immunosuppressant drugs to stop her body rejecting the new womb. However her periods started just three weeks after the operation, a signal that the new womb was working well. Scans showed its lining to be healthy - Doctor Munire Erman Akar said "We can see it from the ultrasound that the endometrium lining is perfect", but added that if she did became pregnant "there are many risks like congenital anomalies because of the immunosuppressive (drugs), and intrauterine growth retardation, preterm labour." Lowering the dose of the drugs is critical for Mrs Sert to carry a healthy baby through pregnancy.
The next step was supposed to be an IVF procedure - planned for September 2012 - when up to two of the eight embryos created from Mrs Sert’s eggs and her husband’s sperm, and frozen ahead of the transplant, will be inserted into her womb. However no information has been published about this, and on 18 September 2012 the Gothenburg team announced their latest advance, stating that:
|
|

A team of researchers at the University of Gothenburg performed the world’s first mother-to-daughter uterus transplantation. The procedure was completed without complications. ... On September 15-16 [2012], a team of researchers, physicians and specialists from the University of Gothenburg performed the world’s first mother-to daughter uterus transplantation, when two Swedish women received new wombs donated by their mothers. ...The first patient had her uterus removed many years ago because of surgery for cervical cancer; the other patient was born without a uterus. Both women, who are in their 30s, have undergone IVF-treatment well before transplantation. ... The aim of the uterus transplant research project is to enable women who had their uterus removed at a young age due to cervical cancer or who were born without a uterus to receive a new womb through transplantation"

Both donating women started in-vitro fertilization before the surgery, and frozen embryos could be thawed and transferred to transplanted uterus' if the receiving women are considered in good enough health after a year-long observation period. "We are not going to call it a complete success until this results in children," said Michael Olausson, one of the Swedish surgeons.
In January 2014, Dr Mats Brannstrom and the
Uterus Transplant Project
at the Sahlgrenska University Hospital Women's Clinic in Gothenburg revealed that the team had conducted nine womb transplants on women who were born without a uterus or had it removed because of cervical cancer. All the transplants were from living relatives. Most of the women are in their 30s and are part of the first major experiment to test whether it is possible to transplant wombs into women so they can give birth to their own children. The transplant operations did not connect the women's uteruses to their fallopian tubes, so they are unable to become pregnant naturally. But all who received a womb have their own ovaries and can produce eggs to be used for IVF treatment.
In October 2014, one of these women become the first in the world to have a baby after having a womb transplant. The 36-year-old mother, who was born without a uterus, received a donated womb from a friend in 2013 last year. Professor Brannstrom described the birth as a moment of "fantastic happiness". Two further women had given birth by the end of November 2014.
Lab-Grown Vagina's

The photos show a uterus 'scaffold' being built, cells incubated, and muscle cells being attached to the growing womb before another incubation and eventual implant.
|
A major advance occurred in early 2014 when doctors at Wake Forest Baptist Medical Centre in North Carolina, USA, announcing that they had successfully grown and implanted vaginas for four teenage women born without vagina's in a four stage process:
|
| Scans of the woman's pelvic region were used to design a tube-like 3D-scaffold for the patient. |
| A small tissue biopsy was taken from the poorly developed vulva and grown to create a large batch of cells in the laboratory. |
| Smooth muscle cells were attached to the outside of the scaffold and vaginal-lining cells to the inside. |
| The vaginas were carefully grown in a bioreactor until they were suitable to be surgically implanted into the patient. |
After surgery, the woman all reported normal levels of "desire, arousal, lubrication, orgasm, satisfaction" and painless intercourse. Although they still can't become pregnant through normal intercourse, IVF is a real possibility. The technique seems to be totally applicable to transwomen, the main issue is the source of the tissue. Penile tissue is preferable, but it may not be obtainable from a post-SRS woman. A biopsy from the uterus of a close female relative is a second option.
A third option is the use of stem cells -
undifferentiated
biological cells
that can
differentiate
into specialized cells. Ten years ago the use of stem cells to create a uterus was pure science fiction, now it is a serious possibility, indeed for a transsexual women this probably the most likely and preferable approach.
Genetically XY Women Gives Birth
2014 culminated with news from the UK of another huge medical advance that will give serious hope to many transsexual women. On Christmas Eve, Hayley Haynes, age 28, gave birth to twin girls - Avery and Darcey. This sounds rather mundane, but it made headlines around the world because nine years earlier Hayley had discovered that she suffered from complete
androgen insensitivity syndrome
(AIS). She was (and still is of course) genetically XY male, and lacked internal female sexual organs such as ovaries or a uterus (aka a womb). As a child there was never any doubt (physically or mentally) that she was anything but a girl, puberty seemed to start normally as her body rounded out and her breasts developed - but she became increasingly worried that her menstruation cycle had not started, i.e. she was not having periods. After growing up dreaming of becoming a mum it was a devastating blow, she says: “When they told me I had no womb I was so confused I felt sick. My biggest fear was never having children."

Encouraged by her boyfriend Sam, Hayley sought help from the NHS. A scan by a specialist at Royal Derby Hospital in 2007 found that Haley had the tiny beginnings of a uterus that had never developed, although just a few millimeters in size it gave hope. Haley was prescribed a cocktail of estrogens and progesterone hormones to create an environment where her uterus could grow. Astonishingly it did, and in 2011 Hayley was informed that she was now able to have IVF. Unfortunately the NHS refused to conduct this procedure for free; Hayley and Sam (now her husband) reluctantly decided to pay £10,500 (about €12,000 or $16,000) to have the procedure performed by a clinic in Cyprus. 13 eggs were taken from a donor mother similar in appearance to Hayley and two were successfully fertilized using Sam's sperm. These were implanted in Hayley's uterus and six weeks a scanned showed that she was pregnant with non-identical twins! The next twelve weeks were nerve-racking as it was vital at this early stage in the pregnancy that Haley took pills to create and accurately simulate the hormone profile of pregnant woman - one day she forgot some pills and briefly feared the worst.

Hayley with her two new-born babies, Darcey and Avery, whom she breast feeds.
|
Thankfully everything went well and in December her doctors decided to induce her two weeks early. On Christmas Eve she gave birth naturally (another minor triumph) to Avery, at 5lbs 3oz, and Darcey, 4lbs 6oz. Although they were slightly premature, the girls were healthy.
Hayley told
Irish Mirror
newspaper: “Becoming a mother was the single most amazing moment of my life. When I held the babies in my arms for the first time I was overwhelmed. I had spent nine years coming to terms with the fact this might never happen, but in that moment all the pain just washed away. "Darcey and Avery are the most beautiful little girls in the world."
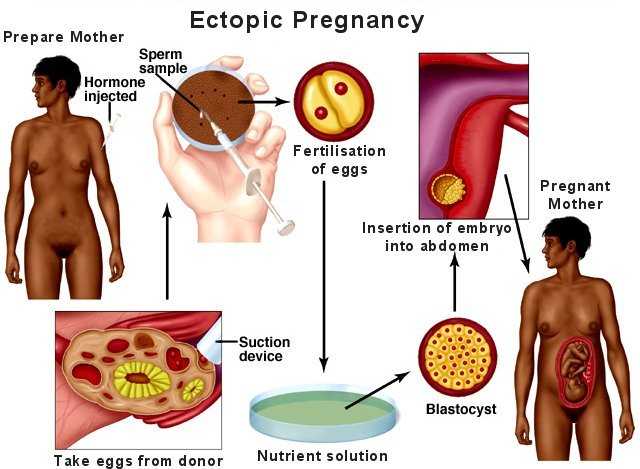
Ectopic Pregnancy
|
Ectopic pregnancy - the development of the baby outside the uterus (womb) - is another possible approach for transsexual women seeking to become pregnant. Natural occurrences of ectopic pregnancy do a occur, however they are considered very dangerous to the mother and subsequent live births are very rare (one pregnancy in millions). Interest in this procedure had faded significantly since 2000 because of the big risks it involves for the patient, and huge the advances made in other areas
However it is still possible that that it might be used for transsexual mothers because of its initial simplicity - no difficult transplants of a uterus or other organs.
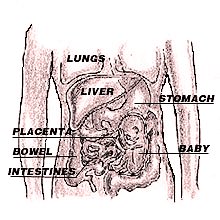
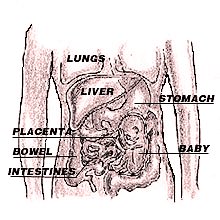
The technique would involve attaching the fetus (the term used for developing babies under 8 weeks from conception) to the muscles inside the transsexual woman's abdomen, or even fashioning a [disposable] artificial womb from abdominal tissue. Attachment to the bowel, with its good blood supply, is another attractive option, but perhaps the worst in terms of post delivery trauma.
Preliminary female hormone treatment will be vital for supporting and encouraging the fetus' placenta to produce enzymes which then eat into whatever internal organ it is placed on, so that the placenta can attach and tap into the blood vessel to obtain nutrition. The baby will then develop inside the woman's abdomen, and the woman will carry the baby for its full term before giving birth by caesarean section.

Sustaining the pregnancy will require further large amounts of female hormones to be taken, in particular high levels of estrogen and progesterone must be maintained during the first three month of pregnancy. The feminizing effects of these may be a problem for a man who wants to become pregnant but doesn’t wish to develop breasts, but it's hardly a problem for a MTF transsexual woman who takes such hormones every day of her life!
There are though two main catches to this procedure:
| Firstly, there is a severe risk of a massive hemorrhage (copious bleeding from damaged blood vessels) when the ectopic ruptures; this is actually the most common cause of women dying in pregnancy. |
| Secondly, if the fetus is implanted in a place where it can thrive without killing the mother, then it can grow to the point where it is a viable baby and can be delivered surgically. However, this leaves the big problem of what to do about the implantation site. While the uterus is designed to cope with the eight-inch wound left when the placenta separates; other organs have no mechanism for helping the placenta to separate and then contracting around themselves to stop the bleeding. Current medical practice with genetic women is to cut the umbilical cord close to the placenta and leave it inside the uterus. If all goes well, it will eventually shrink and be reabsorbed, however with transsexual women there would be a serious risk of infection and other complications with this approach, and surgical removal may be the marginally better option. |
There is a real possibility that the mother will require urgent life saving surgery, either during her pregnancy, immediately after the caesarean, or during the recovery period afterwards.
Procedure
Assuming the mother and her medical team have determined that the risks are acceptable, the exact process for an ectopic pregnancy is:
Step 1: Hormones
Suitable doses of female hormones are administered to make the transsexual woman receptive to the pregnancy.
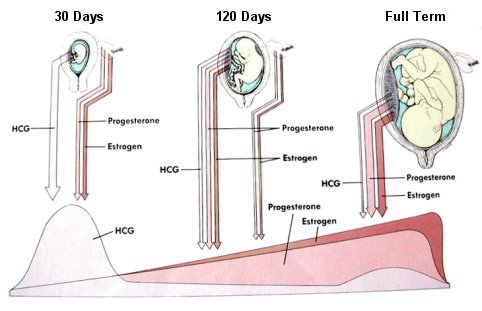 Hormone levels in a woman during pregnancy, after steadily building up for 9 months,
progesterone and estrogen levels drop precipitously after the birth.
Hormone levels in a woman during pregnancy, after steadily building up for 9 months,
progesterone and estrogen levels drop precipitously after the birth.
Step 2: Implantation
IVF (in vitro fertilization) techniques are used to obtain and fertilize egg(s), and then induce an ectopic pregnancy by implanting an embryo and its placenta into the abdominal cavity, into or just under the peritoneum. The peritoneum is the smooth serous membrane which lines the cavity of the abdomen, it surrounds the large interior organs and forms a nearly closed sac.
|
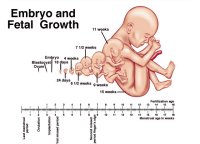
Step 3: Embryo Growth
Once implantation is complete and the embryo is established, hormone treatment can be reduced because the pregnancy itself will take over. The embryo secretes sufficient hormones to maintain its own growth and development.
|
Step 4: Growth of the Fetus
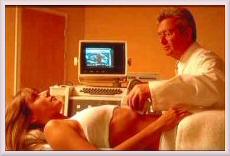
The fetus will be carefully monitored during its development, i.e. fetal heart monitoring, chronic villus sampling, ultrasound scanning, and a constant watch kept over the mother's health.
|
Step 5: Delivery
The delivery will requires open surgery (Caesarean section) to remove the baby and the placenta. Removal of the placenta is the real danger because it forms such intimate connections with surrounding vessels that a massive hemorrhage is likely. Implantation may have also involved other structures in the abdomen, including the bowel and it is possible that parts of other organs may need to be removed.
|



Genetic Parentage
|
Up until our current time, embryos have always been formed by the union of a sperm (supplied by a XY male) and an egg or ovum (supplied by a XX female). Both the sperm and the ovum provide DNA, but the ovum also provides a “house” in which the embryo grows during the early stages of development. An ovum is therefore absolutely essential for reproduction.
A post-SRS transsexual woman faces two major problems in passing her genes on to a child, regardless of whether this is to be carried by a surrogate mother or [in the future] by the transsexual woman herself. Firstly she lacks her own ovaries to produce ovum containing her genes, and secondly having a baby with her husband or a male partner would involve the genetic union of two males - known as "same-sex parenting".
One method for providing the embryo to be implanted is to obtain an egg from an unrelated woman and have it fertilised by sperm from the husband or partner. But while this method is already occasionally used (the baby being carried to term by a surrogate mother), this approach is unsatisfactory for transsexual woman as she has no genetic relationship with her baby.

However, there are several other options that a transsexual woman can take in order to be genetically related to her baby:
If possible, before sex re-assignment surgery, she could have a sperm sample frozen, indeed nearly half of MTF transsexual patients now make this provision before their SRS. The unfrozen sperm could then be used to fertilize a donated ovum (egg) from an unrelated woman. The mother would then have normal 50% shared genes with the baby, but unfortunately the husband/partner would have no genetic relationship unless the ovum came from a close female relative such as a sister.
|
| If no sperm sample is available, then the transsexual's sister or even her mother could donate an ovum for fertilization by the father - in this instance the transsexual mother will share 25% of her babies genes, and her husband/partner a normal 50%. |
|
In the next few years there may become available several new and exciting options which use a cloning technique called "membrane fusion" to create a fertilizable egg:
|
An unrelated woman donates an ovum. The nucleus, containing this woman's DNA, is removed, and an "X" bearing nucleus from one of the transsexual woman's sperm (again frozen from a sample taken before SRS) is put in to its place, creating an unfertilized egg. The new ovum can then be fertilized by the father's sperm and both the mother and her husband/partner will have a normal 50% share of the baby's gene's.
|
Several research teams have reported successes in creating such reconstituted or "hybrid" human eggs, although none have [publicly at least] so far been fertilized for legal reasons - indeed there is a real possibility some countries will make this type of research illegal.
|
An unrelated woman donates an ovum. The nucleus, containing this woman's DNA, is removed, and a nucleus with two sets of chromosome from one of the transsexual woman's cells is put in to its place. Half the genetic material is removed, creating an unfertilized egg with just one set of chromosomes. The new ovum can then be fertilized by the father's sperm and both the mother and her husband/partner will have a normal 50% share of the baby's gene's.
|
|
|
1. Nucleus from a cell of the transsexual woman is removed and transplanted into a donor egg cell from another woman.
2. The hybrid egg cell which now contains the genes of the transsexual woman is fertilized.
3. Transsexual mother is implanted with the embryo, becomes pregnant and eventually gives birth.
|
And finally, the most advanced and technically challenging option of all:
| Human embryonic stem cells are developed in the laboratory into primordial germ cells, a form of cell that can subsequently become follicle eggs (or sperm). This approach potentially allows an engineered egg to produced from a transsexual woman. |
Research
with mice has confirmed that the first steps are possible, although many obstacles remain.
Approach 4 is perhaps the most promising in the short- to medium-term. On 5 Sept 1999 the UK's
Sunday Times
reported a major advance by a team headed by Zev Rosenwaks at the Cornell University Medical Center, New York. They had been able to take immature egg cells from the ovaries of a donor, remove the nucleus (containing the donor's genetic material) and replace it with genetic material taken from
an ordinary body cell
of another animal. The researchers have found they can reprogram the DNA genetic blueprint from any living cell to make it behave like an unfertilised egg. The donor egg cell thus acts as an "envelope" for the prospective genetic mother's genetic material. Once the reconstituted egg cell is mature, it could be fertilized in the laboratory using IVF techniques and the embryo then implanted in to the womb or abdomen of the mother. Rosenwaks said: "We are primarily working with animals, but the work is also being pursued in humans. We have no human pregnancies yet.".
In June 2001 the fertility researchers from Cornell University
reported
that they had now created viable manufactured human eggs using human eggs donated by women undergoing in-vitro fertilization. The experimental procedure uses genetic material from a cell taken from the infertile woman and transplants that material into a donor egg, which has had its genetic material removed.

Florencia de la Vega
was born in Argentina as Roberto Carlos Trinidad, officially in 1976. She transitioned c.1993 and eventually had considerable success as an actress. She had SRS in 2010 and married the following year. Using the husbands sperm and surrogate mother, they had twins (a boy and a girl) in August 2011. The "photo" (left) of Florencia pregnant is presumably photoshopped but amazingly this is not mentioned by the magazine (right).
|
The process is somewhat similar to the cloning technique that was used to create Dolly, the first cloned sheep. There is, however, a crucial difference: Cornell is using only half of the genetic code contained in the adult cell - that of the mother. All adult cells carry two sets of chromosomes, one from the mother and a second from the father, so half have to be removed before fertilization can occur. To do this, the researchers harness the natural ability of the egg to make this happen, using a tiny electrical current, or chemicals, to activate the process of splitting the normal cell's nucleus in half. One half is then taken away so that the reconstructed egg will - according to Professor Palermo, who an assistant professor at the Center for Reproductive Medicine and Infertility at Cornell University Medical Center - "closely resemble a natural, mature human egg", which has only one set of chromosomes. However success rate is low, out of 200 attempts, 17 of the eggs were "haploidised" or made to have the correct number of chromosomes.
The second set of chromosomes will come from the fathers sperm, which also only carries a single chromosome set. To fertilize the eggs, sperm would have to be injected through the cell wall just before the electric shock. The Cornell team has not tried human eggs, but has tried fertilizing artificial mice eggs with some success.

Clearly great progress is being made with this technique which offers considerable hope to transsexual women, but there are still some major potential problems. If sperm is not available then there is concern that using "old" DNA from cells in the mother's body could mean that the new-born baby was the genetic age of the mother. Studies of Dolly the sheep, the first animal to be wholly cloned, suggested that her cells were much older than her chronological age - she prematurely suffered from many medical problems normally associated with old age, and finally had to be put down in 2003 while still relatively "young". Also, some genes are chemically labelled as coming from the mother or the father - a process called "imprinting". These labels would have to be changed, otherwise the resulting embryo would be defective. Finally there are problems with the sex chromosomes, it is possible to produce embryos with an abnormal set of sex chromosomes and it would for example be necessary to screen the individual sperms to make sure the right combination of sex chromosomes was used. But this would have the bonus of letting the couple choose whether to have a son or a daughter.
Dr Ursula Eichenlaub-Ritter, who is a professor of gene technology at the University of Beilefeld in Germany, says that Palermo's technique has the same problems as cloning: It requires many, many failed experiments before a viable egg is produced. She says that she doesn't think the technology is an efficient way to produce this kind of egg.... "I don't see success in the near future.". Dr Palermo thinks that clinical trials on human women are perhaps still 5 years away.
It has become clear (as of June 2002) that the increasingly common animal clones are subject to various genetic problems. It is also expected that while humans may well be cloned imminently, the resulting progeny will be subject to similar problems. There is also no reason to believe that the cloning related reproductive techniques just described above won't suffer such problems. However, it is also reasonable to expect that improvements in cloning techniques and new procedures will eventually overcome these issues.
The Future Is Now
|
When the first version of this page was drafted in 2001, the idea of a genetically XY male-to-female transsexual becoming pregnant was still close to science fiction. Fifteen years later, successful uterus transplants by Dr Brännström's team at the Sahlgrenska University in Sweden, plus the birth of twins by Hayley Haynes in the UK show that all the medical barriers have now been overcome. Given the likely 'no publicity' preference of patients, it is quite possible that in mid-2016, somewhere in the world a transsexual woman was pregnant, or had even already given birth.
|
One huge problem though is the cost. We are still far closer to the first ever headline making heart transplant operation than the 'just' major surgery that it has become. Even when uterus transplants have also become 'just' major surgery, a reasonable estimate is that there will be at least £/$ 500,000 of medical costs for a transgender woman who becomes pregnant once. Few public health services or health insurance policies are likely to cover this procedure, so pregnancy may become the privilege of only transgender women with substantial financial means.
|
Copyright (c) 2016, Annie Richards
Last updated: 11 May, 2016

 One study found that transsexual women are as likely to have reproductive dreams and daydreams as any other women.
One study found that transsexual women are as likely to have reproductive dreams and daydreams as any other women. Famous models and actresses often flaunt their pregnancy in the media
- unfortunately causing distress for some infertile women
Famous models and actresses often flaunt their pregnancy in the media
- unfortunately causing distress for some infertile women 










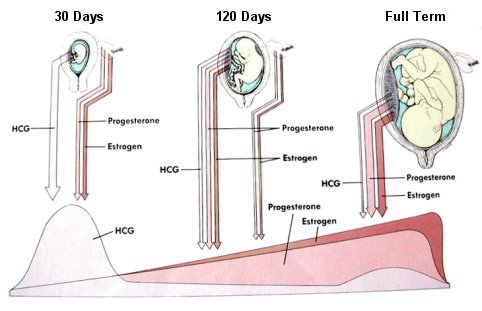 Hormone levels in a woman during pregnancy, after steadily building up for 9 months,
progesterone and estrogen levels drop precipitously after the birth.
Hormone levels in a woman during pregnancy, after steadily building up for 9 months,
progesterone and estrogen levels drop precipitously after the birth.